Background
Tumor Lysis Syndrome (TLS) is an oncological emergency caused by massive tumor cell lysis resulting in hyperuricemia and electrolyte abnormalities which can lead to acute kidney injury, arrhythmias and even death. Most cases of TLS occur after the initiation of cytotoxic chemotherapy in high grade lymphomas and acute lymphoblastic leukemia. Although prevention is the best treatment, once diagnosed, the management of TLS includes supportive care which can be resource intensive. We hypothesized that with improvements in supportive care and the introduction novel drugs including rasburicase, the outcomes for TLS in hematological malignancies have improved in the recent years.
Methods
We used the 2010-2014 National Inpatient Sample database, which is the largest publicly available all-payer inpatient database in the US, to identify patients ≥18 years with primary and secondary diagnoses of TLS (International Classification of Diseases, 9th Revision, Clinical-Modifications [ICD-9-CM] code 277.88) and hematological malignancies. Annual incidence of TLS, mortality, length of stay, costs were calculated for each year 2009-2014, fitted into a log-linear model and compared using Monte Carlo permutation test to study the changes in trend. Statistical analyses were done using STATA version 13.0 and Joinpoint Regression Program version 4.5.0.1.
Results
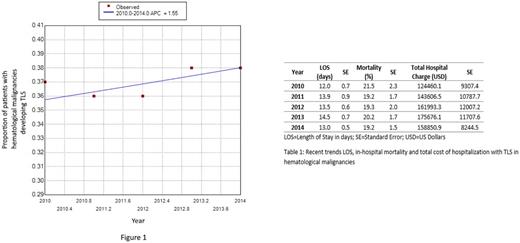
A total of 15,051 cases of TLS were identified among 40,494 patients with hematological malignancies during the study period. The percentage of patients with hematological malignancies who developed TLS was unchanged at 37.1% per year with an annual percent change (APC) of 1.6 which was statistically not significant (95% CI -1.2 to 4.4, p=0.2). Similarly, there was no significant annual change in the in-hospital mortality (19.8%), length of stay (13.4 days) and total hospital charge ($152,917; cost adjusted for yearly inflation using Consumer Price Index, Bureau of Labor Statistics) (Table 1).
Discussion
Our results show that despite widespread availability of rasburicase and improving supportive care, annual incidence of TLS has not changed significantly in the past five years. Similarly, TLS outcomes in hematological malignancies in terms of in-hospital mortality, LOS and cost of hospitalization have also remain unchanged. Strategies to further improve the prevention and outcomes of TLS patients are urgently warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.